The following information is designed to assist Medical Professionals on how to manage a suspected concussion or diagnosed concussion in Community Rugby League. The National Rugby League takes the welfare of its participants at all levels seriously, and if there is any doubt, the player should be treated as having a concussion.
1. Introduction
Sport-related concussion is a traumatic brain injury caused by a direct blow to the head, neck or body resulting in an impulsive force being transmitted to the brain that occurs in sports and exercise-related activities. Symptoms and signs may present immediately, or evolve over minutes or hours, and commonly resolve within days, but may be prolonged.
The NRL’s Community Rugby League Policy and Guidelines for the Management of Concussion which provides an awareness in recognising the signs and symptoms of concussion, the appropriate management of a suspected concussion and the return to learn (RTL) and return to sport (RTS) strategies once a concussion has been diagnosed.
The NRL’s Community Concussion Policy is based on the Consensus Statement on Concussion in Sport released following the 6th International Conference on Concussion in Sport – Amsterdam 2022.
2. Why has the Player been referred for Medical Assessment?
In Community Rugby League there is no requirement for a medical professional to be present at a game. However, Rugby League has a policy which ensures that there is a First Responder at each game who has been taught how to recognise if a player is showing any signs and symptoms of concussion.
A player who exhibits any signs and symptoms of concussion at a game or training session is immediately removed from participating in that activity and referred to a medical professional for assessment. The player can only return to unrestricted training or games when they have been medically cleared.
Upon referral, the player will receive a copy of all the observed signs and symptoms which will assist you as the medical professional with your assessment.
3. How to complete the NRL Medical Clearance Form.
Signs and Symptoms Record
A player who presents for a medical assessment following a suspected concussion should provide you with a copy of all the signs and symptoms observed at the time of injury which will assist with your assessment. This can be in digital or paper format and will look like the screenshot below:

Initial Assessment
Based on your assessment as the Medical Professional you will be required to either clear the player of concussion or diagnose the player with a concussion. Please complete the relevant section outlined in red of the NRL Community Head Injury/Concussion Medical Clearance form as shown below:
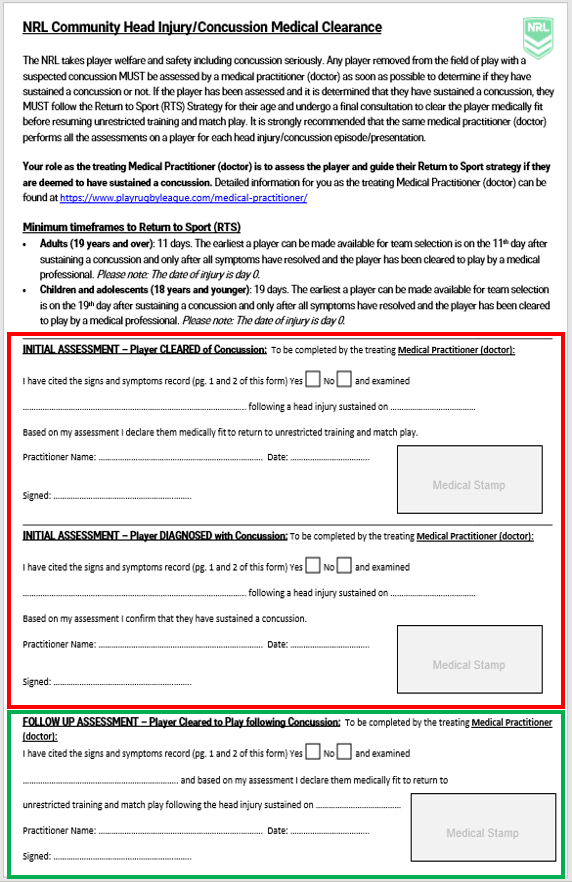
Follow up Assessment.
Any player who has been diagnosed with a concussion must complete a Return to Sport Strategy. Once a player has completed ‘Step 4 – Non-Contact Training Drills’ of the Return to Sport Strategy they need to be cleared to resume unrestricted training and games.
To clear a player to return Sports following a diagnosed concussion please complete the section outlined in green above.
Click here to download the NRL Community Head Injury Medical Clearance Form.
4. Assessment tools for Medical Professionals
The International Concussion in Sport Group has developed a number of assessment tools for Medical Professionals to assist in their assessment of a person with a suspected concussion.
Sport Concussion Assessment Tool 6 (SCAT6)
The SCAT 6 is a standardised tool for evaluating concussions designed for use by health care professionals. It is intended for use in the acute phase of injury, ideally within 72 hours and up to 7 days post injury.
- SCAT6 – For people 13 years and older
- Child SCAT6 – For people between 6-12 years of age.
Sport Concussion Office Assessment Tool 6 (SCOAT6)
The SCOAT6 is a tool for evaluating concussion in a controlled office environment by health care professionals typically from 72 hours following a sports-related concussion.
- SCOAT 6 - For people 13 years and older
- Child SCOAT6 - For people between 6-12 years of age
5. Return to Sport (RTS) Strategy
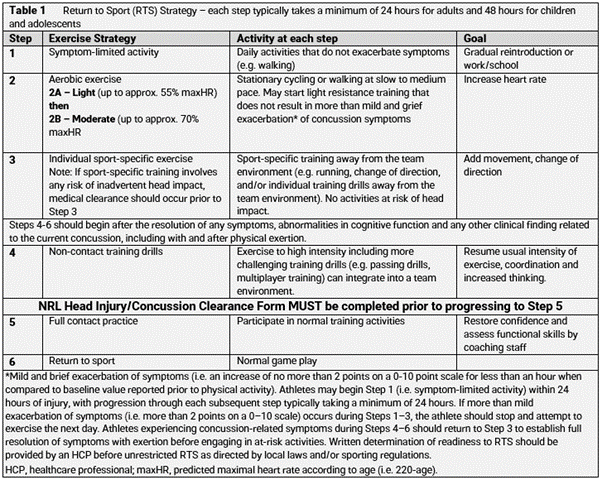
Rehabilitation after a concussion should be supervised by a medical practitioner and should follow the stepwise symptom limited progression as outlined in Table 1 below.
Relative Rest
All players who have sustained a concussion should complete an initial period of relative rest in the first 24-48 hours post injury. Relative rest includes reduced screentime, activities of daily living and light intensity physical activity (e.g. walking) that does not exacerbate symptoms.
Adults v Children and Adolescents
For adults, each stage in the RTS Strategy should be a minimum of 24 hours’ duration, meaning a period of 7 to 8 days is the minimum time frame that an adult could potentially be cleared to return to unrestricted training. This does not mean return to play, as an adult cannot RTS until the 11th day after sustaining a concussion.
For children and adolescents, each stage in the RTS Strategy should be a minimum of 48 hours’ duration, meaning a period of 14 to 16 days is the minimum time frame that a child or adolescent could potentially be cleared to return to unrestricted training. This does not mean return to play, as a child or adolescent cannot RTS until the 19th day after sustaining a concussion.
Longer return to sport timeframes are recommended in community sport settings. Contact training should only be attempted after the completion of Step 4 of the RTS strategy and only after a final doctors’ assessment and clearance using NRL Community Head Injury/Concussion Medical Clearance Form.
6. Return to Learn (RTL) Strategy
Concussion in children and adolescents can cause problems with memory and processing of information, which interferes with their ability to learn in the classroom. In this instance a RTL Strategy may be required. If symptom exacerbation occurs during cognitive activity or screen time, difficulties with reading or other aspects of learning are reported, clinicians should consider the implementation of the RTL Strategy at the time of diagnosis and during the recovery process. When the RTL Strategy is implemented, it can begin following an initial period of relative rest with an incremental increase in cognitive load as per Table 2. While the RTL and RTS Strategies can occur in parallel, full RTL should be completed prior to unrestricted RTS.
7. Timeframes to Return to Sport
Any player who is diagnosed with a concussion cannot return within the timeframes outlined below:
- Adults (19 years and over): Eleven (11) days. The earliest a player can be made available for team selection is on the 11th day after sustaining a concussion and only after all symptoms have resolved and the player has been cleared to play by a medical professional.
- Children and Adolescents (18 years and younger): Nineteen (19) days. The earliest a player can be made available for team selection is on the 19th day after sustaining a concussion and only after all symptoms have resolved and the player has been cleared to play by a medical professional.
8. Multiple or concerning concussions.
When a player:
(i). Has sustained two (2) diagnosed concussions within the previous three (3) months, three (3) concussions in a 12-month period, or, has persistent concussion symptoms (>28 days) or an unusual presentation; or
(ii). Over time (not just within a 12-month period):
• Is developing concussion symptoms with less force; or
• Is experiencing progressively increasing length of concussion symptoms; or
• Has an increasing symptom load (a greater number of concussion symptoms); or
• Has a decreasing time period between concussive / possible concussive events; or
• Has significant mental health issues (e.g., anxiety, depression) potentially related to head injuries, then,
The NRL requires that the player be formally sent for assessment with a specialist (Neurologist, Neurosurgeon or Sport and Exercise Physician) who has a recognised interest in sport related concussion management (Concussion Specialist) as part of a multi-disciplinary team approach. The assessment should also include formal neuropsychological testing if recommended by the Concussion Specialist providing the opinion. This should occur to ensure the player has fully recovered from their concussions, to assess the risks of further concussions and to determine whether the player is currently fit to participate in training and/or matches. In this situation the treating specialist may recommend a prolonged period away from contact training and games. Any decision regarding prolonged standdown periods needs to be made after thoughtful deliberations between the athlete, their support persons and the treating specialist. A copy of the Concussion Specialist’s opinion should also be made available to the appropriate governing body on request.
9. Additional information
The NRL also considers the Australian Institute of Sport's Concussion and Brain Health Position Statement 2024.
RELATED ARTICLES
Return to Play - Player Responsibilities
Return to Play - Role of the Sports Trainer
Was this article helpful?
That’s Great!
Thank you for your feedback
Sorry! We couldn't be helpful
Thank you for your feedback
Feedback sent
We appreciate your effort and will try to fix the article